
For Teachers & Professionals
Pregnancy and Sexuality
There has been a long history of misunderstanding aspects of pregnancy, where patients often must rely on anecdotes, old wives' tales, and other unreliable sources of information, and the physicians themselves had misleading knowledge about the topic of the relationship between pregnancy and coitus. In an old piece of a medical journal, we can read that coitus during pregnancy was probably associated with albuminuria and puerperal sepsis: “As far as I can gather, albuminuria and puerperal sepsis are far rarer in the animal than the human world; the only practical difference in the two pregnancies is that coitus does not take place in the former and it does in the latter.” In another article from 1929, we read that: “It is advisable to prescribe moderation in sexual intercourse between the sixth and eight months, and complete abstinence after the eighth month”. Another quotation that provides a historical perspective on the matter is taken from an obstetrician’s journal: “There are many reasons for forbidding coitus during gestation: first, the danger of abortion, which is caused by the impact of the penis against the cervix. Second, the nervous shock is not well borne by a woman whose nerve energy is already overtaxed. Third, animals do not copulate when the female is pregnant, it would be wise for him (man) to follow their instincts. Fourth, the danger of infection. The danger from coitus is greatest in the first three months when usually the fact of pregnancy is not always sure, and in the last three months, when the abdominal tumour is large and the element of infection more prominent. It is wise to restrict the practice to the intervening months, or better, advise against it entirely”.
Almost a century has now passed, but culture and history are the reason why some myths may still persist in our minds. Some studies found that at least half of pregnant women believe that intercourses are bad for the foetus. A lot of people still think that having sex during pregnancy might lead to preterm labour and even physicians, unless they are familiar with the scientific data in the area, have the potential for providing patients with misleading or incorrect information.
A more open discussion between clinicians and patients about sexual activity during pregnancy is relevant and may help to alleviate women’s fears, close knowledge gaps and reassure those who wish to be sexually active throughout pregnancy. As an ob/gyn, approaching sexual health in pregnancy requires both an understanding of physiological changes that can occur and attention to culturally sensitive issues that may arise. Throughout the antepartum and postpartum periods, clinicians have the opportunity to provide direct counselling about sexual activity as well as to affect patients’ intimate partner relationships indirectly. This article should provide a basis on which physicians can better inform both themselves and other healthcare providers under their direction.
1. PHYSICAL ASPECTS OF SEXUALITY IN PREGNANCY
This is probably the most visible aspect. Nausea and vomiting during early pregnancy can prevent a woman from expressing her sexuality paradoxically at a time when the couple as a unit might feel the closest. Fatigue is another factor influencing the first and last trimesters. Urinary frequency and urgency can become hindrances to sexual response, as can constipation, fetal movement, and back pain. Women might release milk during sexual activity and have augmented vaginal secretions that may inhibit the partner.
Painless, short-lived, pinkish, brown, or light red spotting after sex is also a normal response to changes in the cervix, especially in the first few months. Since the cervix becomes more sensitive during pregnancy, a small amount of bleeding can occur if the cervix is bruised during deep penetration. An uninformed couple can be alarmed by unexpected postcoital bleeding.
Vasocongestion during arousal might last longer and cause discomfort, while orgasm may be accompanied by cramping or muscle spasms. General physical discomfort is the most prevalent reason to avoid sexual intimacy.
2. PSYCHOLOGICAL ASPECTS OF SEXUALITY IN PREGNANCY
Sexuality is affected by many factors, among them environmental, interpersonal, and intrapersonal factors. Sexual performance can be inhibited by a lack of knowledge or by anger, fear, and other potentially negative attitudes. Pregnancy can be a stressful period for the mother but also for the couple, and this might have a negative impact on sexuality. The importance of sexuality and intercourse may diminish. Pregnancy can precipitate psychological problems in a woman that have not previously arisen: recollections of childhood rivalries with siblings or her own mother or conflicts about her role as a woman, or the sudden position of need. A major concern for a woman is her perceived loss of attractiveness, and this correlates positively to coital activity and sexual enjoyment. A man, conversely, must deal with his love for a partner despite her radically altered physique. Either a direct verbalization of disinterest or more subtle avoidance behaviours can reinforce a woman's sense of non-attractiveness. Clear understanding allows the couple to be more open in their communication, making sexual adjustments easier during pregnancy.
3. SEXUAL ACTIVITY IN PREGNANCY
Sexual activity shows a progressive diminishing in desire. A variety of reasons have been suggested for this decrease in sexual activity. Early in pregnancy, some women report fears that intercourse will cause miscarriage; during the third trimester, both mothers and fathers report fears that intercourse or orgasm may harm the fetus. However, there is currently no strong research evidence of increased pregnancy complications associated with sexual activity during pregnancy. Other reasons for decreased coital frequency include physical discomfort associated with intercourse, particularly in the man-on-top position, and loss of interest in sex. Hormonal fluctuations may cause different levels of libido and the consistent reduction in orgasmic function during pregnancy may also be related to changes in physiologic response or to active repression of orgasm to protect the baby. Diminished clitoral sensation appears to be the most common cause of sexual dysfunction followed by loss of sexual interest and orgasmic disorder. The increased need for physical contact, thus non-coital behaviour, should be included in pre-pregnancy counselling. The position used might also change, toward a preference for a side-to-side one.
REFERENCES
Bartellas E, Crane JM, Daley M, Bennett KA, Hutchens D. Sexuality and sexual activity in pregnancy. BJOG. 2000; 107: 964–8.
Brown, C, Bradford, J., et al, (2008)Glob. libr. women's med., (ISSN: 1756-2228) ; DOI 10.3843/GLOWM.10111
DeLee JB: The Principle and Practice of Obstetrics, 6th ed. Philadelphia, WB Saunders, 1934
Cotton F. W. (1930). COITUS IN PREGNANCY. British Medical Journal, 1(3618), 886.
Epitome of Current Medical Literature. (1929). British Medical Journal, 2(3588), E55–E58.
Nwadike, V. R. (2020, May 28). Bleeding After Sex During Pregnancy: Is It Normal? Healthline. Retrieved September 22, 2022, from https://www.healthline.com/health/pregnancy/bleeding-after-sex-during-pregnancy
Share the knowledge!
More For Teachers & Professionals Q&A

Communication Strategies for Discussing PrEP

Chronic Kidney Disease and Sexuality

Teaching consent to Young children (8 – 12 years old)
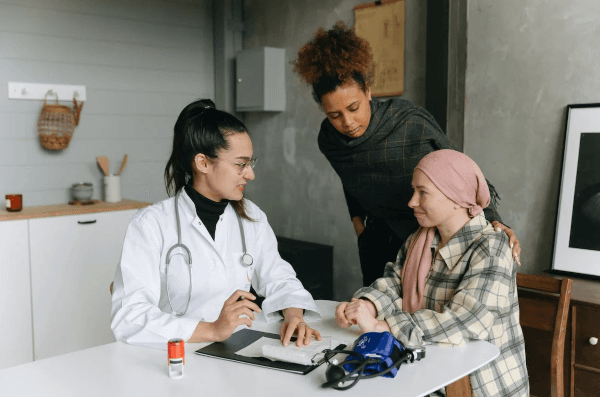
Female cancer and Sexuality Part 1: Clinical inquiry regarding female sexual health
Testicular cancer and Sexuality

LGBTQIA+ Community and Health Care Services
This is a website that WE are building together. If you have a question there is no answer to on this site, send it here!
